Fluorescence imaging systems face a fundamental challenge: detecting signals through tissue, which...
Why Tissue Composition Matters in Fluorescence Imaging
A Deeper Look into Light Interaction
In fluorescence-guided surgery and other medical imaging techniques, understanding how light interacts with tissue is critical. While engineers and physicists often simplify complex systems to approximate solutions, light’s interaction with real tissue involves unique challenges that can affect imaging performance. This post dives deeper into why tissue composition matters and highlights the importance of using optical phantoms that replicate tissue properties.
Simplifying Light and Tissue Interactions
Water is commonly used as an initial approximation for how light might travel through tissue, but tissue composition is much more complex. Take a simple test with your phone’s flashlight on your fingertip: the red glow is visible because red light penetrates further into tissue than blue or green light, which are absorbed or scattered at shallower depths.
This variance in light behavior occurs due to chromophores—substances within tissue that absorb and scatter light in specific ways. Blood, lipids, and water are key chromophores in the body, and each has unique effects on how far different wavelengths of light can travel. For instance:
- Blue and green light are attenuated—or reduced—quickly, so light can only reach superficial layers.
- Red and near-infrared light travels deeper, allowing for more effective imaging of structures below the surface.
Why Chromophores Matter in Imaging
Chromophores in tissue, such as hemoglobin in blood, absorb and scatter light, shaping how deep light can penetrate and how fluorescence signals are detected. In fluorescence-guided surgery, fluorophores are used to tag specific structures or tissues, emitting visible light when excited by an external light source. However, chromophores in tissue can block or reduce this fluorescence signal, especially for fluorophores that emit blue or green light, which are more easily attenuated.
There is an optical window where biological tissues exhibit minimal light absorption and scattering, allowing for deeper penetration of light. This optical window, where red and near-infrared light can travel further, is a key design parameter used to develop optical sensing and imaging systems for medical applications. Engineers use this knowledge to design systems optimized for specific imaging depths and to better predict how effective fluorescence imaging will be under different conditions.
The Role of Phantoms in Simulating Tissue Properties
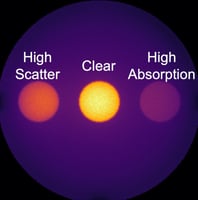
Because tissue is heterogeneous and complex, optical phantoms with tissue-equivalent properties are vital in developing reliable imaging systems. Phantoms are designed to mimic the optical characteristics of tissue, including the scattering and absorption effects of chromophores like blood and lipids. By testing with phantoms, developers can accurately measure system performance under conditions that represent real-world challenges, like light attenuation and fluorescence depth limitations.
Takeaways: Why Tissue Properties and Phantoms Matter for Imaging
- Chromophores Impact Light Penetration: Key substances in tissue selectively absorb and scatter light, affecting imaging depth and clarity.
- Fluorophore Choice Influences Depth Detection: Red and near-infrared fluorophores are ideal for deeper imaging, while blue and green are better for superficial structures.
- Phantoms Enable Realistic Testing: Using phantoms with tissue-equivalent properties helps engineers simulate real-world conditions and optimize imaging systems accordingly.
- Informed System Development: Understanding tissue properties allows developers to anticipate imaging challenges and design more effective fluorescence-guided systems.
The complexities of tissue composition significantly impact fluorescence imaging outcomes. Chromophores within tissues play a pivotal role in determining how far light can travel and how deep fluorescence emissions can be detected. Optical phantoms that replicate these properties provide an invaluable resource, supporting the development of imaging systems that work reliably in the operating room, enhancing surgical precision, and improving patient outcomes.