The FDA recently released draft guidance for optical imaging drugs, including an appendix dedicated...
7th Annual International Congress for Fluorescence Guided Surgery
I recently attended the 7th Annual International Congress for Fluorescence Guided Surgery. This half-day meeting sponsored by the International Society for Fluorescence Guided Surgery (ISFGS) came at the tail end of the IFSO meeting in Miami last month.

In addition to providing an opportunity to interact with some of our customers and other device developers showcasing their imaging systems, it was a great learning opportunity to better understand the clinical workflow. QUEL Imaging was founded based on expertise developed at the Center for Imaging Medicine at Dartmouth College, so our perspective is heavily-weighted towards the engineering and technical aspects of fluorescence imaging. This academic background also means we’ve been working on early stage clinical translation, where some projects and ideas may take another 5-10+ years before clinical adoptions (and reimbursement).
The ISFGS meeting brought together surgeons from across the globe who specialize in fluorescence imaging. The discussions primarily focused around the uses of indocyanine green (ICG) with an emphasis on laparoscopic and robotic procedures. There was consensus among the presenters that improved visualization improves outcomes, with Dr. Luigi Boni stating, “If we have a technology to allow us to see better, we’ll perform better” later going on to say surgeons are more precise when using fluorescence imaging.
Many also agreed ICG fluorescence is useful for surgical training, especially in robotic procedures where the sense of touch and haptic feedback is reduced. For surgeons new to the modality, it was suggested to start using ICG in less complicated procedure to become familiar with it. Overall, multiple reports were presented and group discussions support that ICG helps improve surgeon confidence and reduces complications.
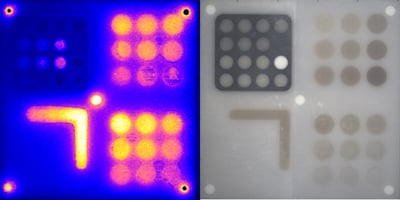
A general desire to use more quantitative visualization was expressed by a number of presenters. Some visualization systems allow the surgeon to determine the ratio or percentage of fluoresce in specific regions of interest relative to a reference area. However, a few presenters said this method sometimes failed, especially when high background fluorescence was present. Determining flow rate for dynamic perfusion assessment was presented as a more promising quantitative alternative since compounding factors such as dosage, timing and administration route can impact static assessments. This is not yet standardized, but ISFGS has done work to compile a list delivery methods by indication.
The session closed with a presentation by Jason Warram, who provided his insight on trends in fluorescence guided surgery from a more academic perspective. New imaging modalities, such as multi-spectral, multi-modal and SWIR were described. The newly approved Cytalux and other targeted probes were presented which lead to an overview of back-table intraoperative pathology. The caveat to these new probes and oncologic applications is they “need most sensitive settings to discern tumor from normal tissue.”